What causes gum disease
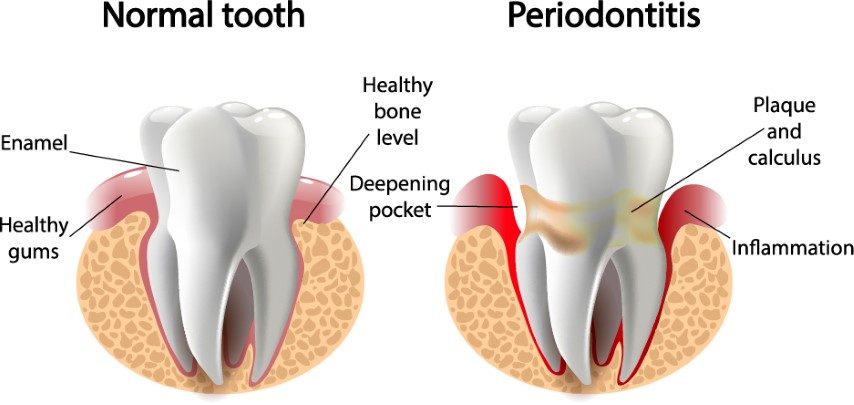
Naturally, mouths are full of bacteria has the ability to form a sticky, colourless “plaque” layer on teeth surfaces. Good oral hygiene and regular visits to the hygienist help get rid of plaque. If plaque is not removed, it turns into hard calculus “tartar” that brushing doesn’t clean. Only a professional cleaning by a dentist or dental hygienist can remove tartar. Two main conditions affect the Gums, the bone and the ligaments that hold the tooth to the bone.

Risk Factors in Periodontitis
Smoking:
Smoking is one of the significant risk factors associated with gum disease. Smokers are four times more likely to have periodontal disease than non-smokers Additionally, People who continue to smoke during the treatment for periodontitis will have up to 50% less healing response than non-smokers.
Hormonal changes:
in girls/women. These changes can make gums more sensitive and make it easier for gingivitis to develop.
Diabetes:
People with diabetes are at higher risk for developing infections, including gum disease.
Other illnesses and their treatments:
Diseases such as AIDS and its treatments can negatively affect the health of gums, as can treatments for cancer and other treatment which requires the suppression modulation of the Immune system.
Medications:
Some medications that can reduce the flow of saliva and without enough saliva, the mouth is vulnerable to infections such as gum disease. And some other medications can cause abnormal overgrowth of the gum tissue making it difficult to keep teeth and gums clean.
Genetic Factors:
Some people are more prone to severe gum disease than others due to inherited factors.
Top Treatments
- General Dentistry
- Preventative Dentistry
- Cosmetic Dentist
- Teeth Straightening
- Missing Teeth
- Restorative Dentistry
- Nervous Patients
Get In Touch

1- Gingivitis
The longer plaque and tartar are on teeth; the more damage the bacteria can cause to the gums. The bacteria cause inflammation of the gums “gingivitis where the gums become red, swollen and bleed easily sometimes just by brushing. Gingivitis is a mild form of gum disease and in most cases, it can be reversed with excellent oral hygiene and regular cleaning by a dentist or dental hygienist. This form of gum disease does not include any loss of bone and tissue that hold teeth in place

2- Periodontitis
Untreated Gingivitis can advance to “periodontitis” effecting the gums, bone and the entire tooth to bone attachment system. In periodontitis, gums spaces (called “pockets”) are formed between the gums and the bone that become infected. If the pockets extend below the gum line the immune system initiate a reaction to fight the invading bacteria which results in the break down the bone and connective tissue that hold teeth in place. If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.
How is Gum Disease (Periodontitis) treated?
The main goal of treatment is to manage and control the disease as it is generally not curable. The number and types of treatment will vary, depending on the extent of the disease. Any type of treatment requires that the patient keep up good daily care at home and changing certain behaviours, such as quitting smoking, as a way to improve treatment outcome. There are two main types of treatment currently available depending on the extend of the disease. Non-Surgical (scaling and root plaining) as a first phase, if no respond or in cases where the damage to the bone and attachment system is severe, surgical management is used.
None Surgical Deep Cleaning
(Scaling and Root Planning) in this phase, the plague is removed through a deep-cleaning method called scaling and root planning. Scaling means scraping off the tartar from above and below the gum line. Root planning removes the deposits along the root service inside the pockets, this helps remove bacteria that contribute to the disease.
Surgical Treatments
Flap Surgery
If Deep cleaning treatment fails to reduce the depth of the pockets around the tooth Surgery might be necessary. Flap surgery is performed to remove tartar deposits in deep pockets or to reduce the periodontal pocket and make it easier for the patient to keep the area clean. This common surgery involves lifting back the gums and removing the tartar and cleaning the area. The gums are then sutured back in place around the tooth again. After surgery, the gums will heal and fit more tightly around the tooth. This sometimes results in a reduction of gums making the teeth longer.
Bone and Tissue Grafts
In addition to flap surgery guided tissue regeneration can be used in severe cases to compensate for lost bone. in this technique, natural or synthetic bone is placed in the area of bone loss, can help promote bone growth. In this procedure, a small piece of mesh-like material is inserted between the bone and gum tissue. This keeps the gum tissue from growing into the area where the bone should be, allowing the bone and connective tissue to regrow. In cases where gum tissue has been lost soft tissue graft can be performed with a synthetic material or tissue taken from another area of the mouth and used to cover exposed tooth roots and defects.
Success Rate
Since each case is different, it is very hard to estimate the success rate of surgical treatments. Treatment results depend on many things, including how far the disease has progressed, how well the patient keeps up with oral care at home, and certain risk factors, such as smoking, which may lower the chances of success. Our team will advise you about your estimated individual success rate along with all risk and benefits.